Measuring Respiration Rate
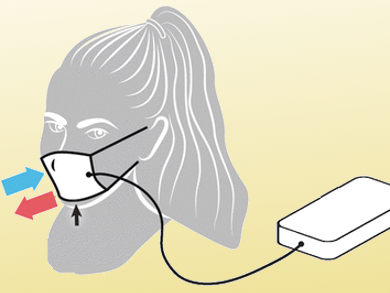
A simple but effective sensor for monitoring the respiration rate of individuals has been created. Taking advantage of the hygroscopic character of ordinary paper, scientists at Harvard University have developed an electrical sensor to detect the periodic changes of humidity by breathing in and out. As they report in the journal Angewandte Chemie, the respiration data can be transmitted to and collected by nearby smartphones or tablet computers for further processing, storage, or transmittance to practical therapists. A simple face mask carrying the sensor system and worn in hospital wards may thus save lives.
A person’s respiration rate often reflects their health status and physical condition. Second- to minute-long pauses in breathing characterize sleep apnea, and breathing too fast at rest can give important predictions of cardiac arrest. Furthermore, athletes count on their breathing as an indication of fitness, favoring slow but deep breaths during exercises.
Low-Cost Paper-Based Humidity Sensor
How can breathing be monitored in a user-friendly, safe, and inexpensive way? Interestingly, there are few practical and cost-effective methods available to detect respiration rates, apart from simply counting the rising and falling of the chest. A team of chemists and bioengineers under guidance of George M. Whitesides have designed a low-cost monitoring system based on a paper patch that hosts the electrodes for the detection of the humidity changes in the paper fibers during respiration. The sensor is incorporated in conventional face masks used in hospitals.
The scientists asked healthy individuals wearing these functionalized face masks to perform exercises at various levels and monitored the sensitivity of the sensor and the reliability of the data. In addition, they explored the conditions at rest by examining normal breath rates, pauses, and random combinations of fast, slow, shallow and deep breaths. The idea behind the system was that extra humidity by exhalation would increase the water layer on the cellulose fibers, while inhalation results in the opposite effect. “Essentially, the paper sensor transduces variations in the level of moisture of its immediate surrounding to an electrical signal,” the authors say.
The amplified and processed data are then transferred from data acquisition electronics to a smartphone or tablet computer running a convenient Android app to display and analyze the incoming data stream. “The system is non-invasive, and thus allows physical scientists access to physiologically relevant human data under simple IRB [Institutional Review Board] approvals,” the authors state. It is the simplicity and the low cost combined with reliability that could make their paper-based electric respiration sensor highly attractive to the healthcare system.
- Paper-Based Electrical Respiration Sensor,
Firat Güder, Alar Ainla, Julia Redston, Bobak Mosadegh, Ana Glavan, T. J. Martin, George M. Whitesides,
Angew. Chem. Int. Ed. 2016.
DOI: 10.1002/anie.201511805