Impermeable Mycomembrane of Tuberculosis Bacteria
Tuberculosis is one of the most widespread life-threatening infectious diseases. Not only does antibiotic resistance make treatment increasingly difficult, but the bacteria’s relatively impermeable mycomembrane also limits the effectiveness of many drugs. In search of new antibiotics, researchers have developed a structural analogue of mycolic acid, the essential membrane building block. This drug blocks key enzymes used in mycomembrane biosynthesis, significantly increasing the effectiveness of conventional antibiotics.
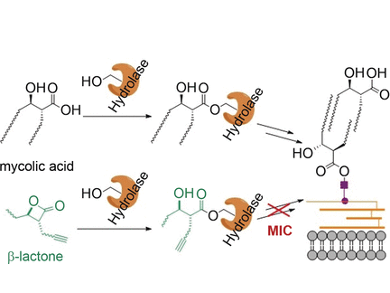
The mycomembrane of the tuberculosis pathogen Mycobacterium tuberculosis is a lipid double-layer that forms an outer barrier. Mycolic acids are a critical component. They are branched β-hydroxylated fatty acids with two long hydrocarbon chains. The biosynthesis of the mycolic acids and their incorporation into the mycomembrane involve a series of critical enzymatic steps in which the mycolic acid molecules are bound to serine groups of various enzymes through ester bonds.
Antibacterial β-Lactone Infiltrates Mycomembrane Biosynthesis
Scientists working with Stephan A. Sieber and Eric J. Rubin thought that molecules camouflaged as mycolic acids would also bind to these enzymes, blocking them and “infiltrating” the membrane biosynthesis process. They chose to test this theory using β-lactones, tensioned four-membered ring containing an internal ester bond. Ring-opening results in a structure that corresponds to the portion of the mycolic acid molecules that bind to the enzymes. The team from the Technical University of Munich, Gemany, the Harvard T.H. Chang School of Public Health, Harvard Medical School, and Texas A&M University, all USA, tested a broad palette of different β-lactones for antimycobacterial activity and hit a bullseye: Compound “EZ120” inhibits the biosynthesis of the mycomembrane and kills off the bacteria.
By using enzyme tests and mass spectrometric studies using special 13C-labelled substrates (metabolite profiling), the scientists demonstrated that the new inhibitor primarily blocks the enzymes Pks13 and Ag85. Pks13 is a polyketide synthase, which links the two chains of the mycolic acids into a single molecule. Ag85 is a group of serine hydrolases that plays a critical role in the incorporation of mycolic acids into the mycomembrane.
EZ120 works in very small doses, is outstanding at entering tuberculosis pathogens, and has low toxicity toward human cells. Administration together with the already authorized antibiotic vancomycin significantly increases the effectiveness of both individual substances. In combination with vancomycin, EZ120 is about 100 times as effective, presumably because weakening of the mycomembrane allows it to more easily enter the bacteria. Taken together with the fact that several cellular target are addressed, this could provide a novel approach for tuberculosis treatment.
- An Antibacterial β-Lactone Kills Mycobacterium tuberculosis by Disrupting Mycolic Acid Biosynthesis,
Johannes Lehmann, Tan-Yun Cheng, Anup Aggarwal, Annie S. Park, Evelyn Zeiler, Ravikiran M. Raju, Tatos Akopian, Olga Kandror, James C. Sacchettini, D. Branch Moody, Eric J. Rubin, Stephan A. Sieber,
Angew. Chem. Int. Ed. 2017.
https://doi.org/10.1002/anie.201709365