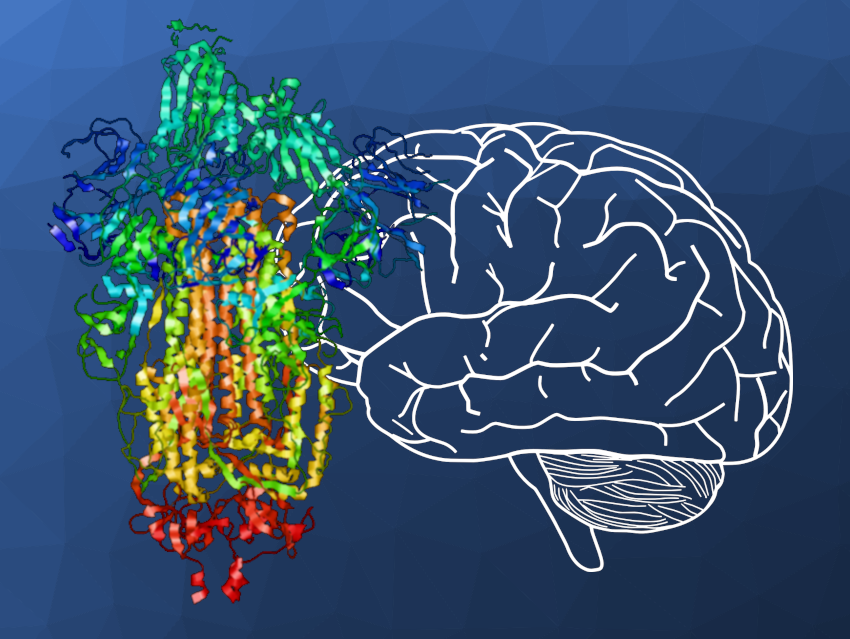
Long-term health issues following COVID-19 (long COVID) pose a major public health concern. Long COVID symptoms include health problems such as fatigue, memory deficits, and shortness of breath. Why even mild cases of COVID-19 can sometimes cause severe long-lasting health issues remains unknown to date. Previous research indicated that in long COVID, it is likely not the SARS-CoV-2 virus itself but viral residues that remain in the body and cause a prolonged response of the immune system, i.e., inflammation. Inflammation is a normal, protective response to infection, but it can have harmful effects when it occurs in healthy tissue or goes on for too long. The spike protein, a protein shed by SARS-CoV-2 that mediates the entry of the virus into the cell, has been connected with inflammation and potential damage to various tissues.
Ali Ertürk, Helmholtz Munich, Neuherberg, Germany, Ludwig-Maximilians-University Munich, Germany, Koç University, School of Medicine, İstanbul, Turkey, and colleagues have detected the spike protein in post-mortem samples from patients who had recovered from COVID-19 but died of non-COVID-19 causes—located in various organs including the brain, the skull, and the meninges, i.e., the connective tissue enveloping the brain and the spinal cord. In mouse experiments, the group injected the spike protein into both healthy mice and into mice that serve as model animals for stroke and traumatic brain injury. They found that this caused inflammation in the central nervous system and worsened neurological damage from brain injury. Together, the results suggest that the spike protein may persist in the brain, where it causes prolonged inflammation and detrimental effects that may lead to neurological issues like memory loss.
The team also found that mice that had been vaccinated with the BioNTech/Pfizer Comirnaty vaccine prior to SARS-CoV-2 infection had lower levels of spike protein in several organs such as the brain and lungs. Thus, vaccination may protect against the retention of spike protein, while not completely eliminating spike protein accumulation after infection. Overall, the persistence of spike protein in organs may contribute to neurological long COVID symptoms. According to the researchers, future clinical studies are needed to investigate the clinical effects of reducing spike protein levels in long COVID patients, in addition to the preventive effects of vaccination.
- Persistence of spike protein at the skull-meninges-brain axis may contribute to the neurological sequelae of COVID-19,
Zhouyi Rong, Hongcheng Mai, Gregor Ebert, Saketh Kapoor, Victor G. Puelles, Jan Czogalla, Senbin Hu, Jinpeng Su, Danilo Prtvar, Inderjeet Singh, Julia Schädler, Claire Delbridge, Hanno Steinke, Hannah Frenzel, Katja Schmidt, Christian Braun, Gina Bruch, Viktoria Ruf, Mayar Ali, Kurt-Wolfram Sühs, Mojtaba Nemati, Franziska Hopfner, Selin Ulukaya, Denise Jeridi, Daniele Mistretta, Özüm Sehnaz Caliskan, Jochen Martin Wettengel, Fatma Cherif, Zeynep Ilgin Kolabas, Müge Molbay, Izabela Horvath, Shan Zhao, Natalie Krahmer, Ali Önder Yildirim, Siegfried Ussar, Jochen Herms, Tobias B. Huber, Sabina Tahirovic, Susanne M. Schwarzmaier, Nikolaus Plesnila, Günter Höglinger, Benjamin Ondruschka, Ingo Bechmann, Ulrike Protzer, Markus Elsner, Harsharan Singh Bhatia, Farida Hellal, Ali Ertürk,
Cell Host Microbe 2024.
https://doi.org/10.1016/j.chom.2024.11.007