In antibacterial photodynamic therapy, irradiation is used to produce reactive oxygen species that kill off bacteria. Because it requires external light and oxygen, this method is only suitable for surface infections. A Chinese research team has introduced a molecular “singlet oxygen battery” that can be “charged” with reactive oxygen, which it then releases in deep tissue layers to target methicillin-resistant staphylococcus.
Treating Antibiotic-Resistant Bacteria with Photodynamic Therapy
Antibiotic-resistant bacteria are on the rise. Though often harmless to healthy people, dreaded multidrug-resistant “hospital pathogens” such as methicillin-resistant Staphylococcus aureus (MRSA) use injuries or fresh surgical wounds to gain entry to the body. They also infect immunocompromised patients. Because antibiotics are not effective, there is sometimes no remedy.
One highly promising alternative is antibacterial photodynamic therapy, which is already widely used in dentistry. In this technique, a light-activated substance (photosensitizer) is irradiated, triggering a photodynamic reaction that produces singlet oxygen (1O2), an excited form of oxygen. Unlike antibiotics, this substance simultaneously attacks multiple biomolecular sites on the bacteria. It is easy to use, safe, painless, and generally free of side effects. Unfortunately, it has only been useful for surface infections because the necessary light only penetrates a few millimeters into the tissue. Additionally deeper tissue layers also do not have enough oxygen for effective treatment.
Improvement with Singlet Oxygen Battery
Bingran Yu and Fu-Jian Xu, Beijing University of Chemical Technology, China and colleagues have developed a new approach to photodynamic therapy: a “singlet oxygen battery” that can be used to fight deep bacterial infections because it requires neither light nor external oxygen.
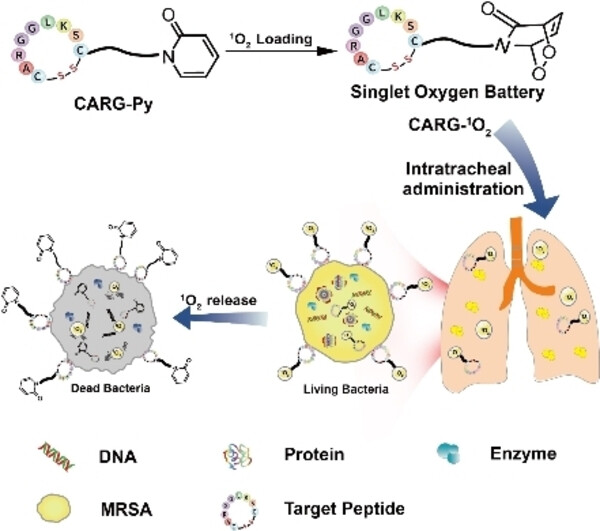
As shown in the picture, the conversion of oxygen into reactive singlet oxygen through irradiation in the presence of a CARG-Py that captures light (photosensitizer) happens first. It produces singlet oxygen over a time course of approximately 30min. The “battery” is “charged” with the singlet oxygen (“singlet oxygen battery” CARG-1O2) and can release singlet oxygen without external irradiation or oxygen.
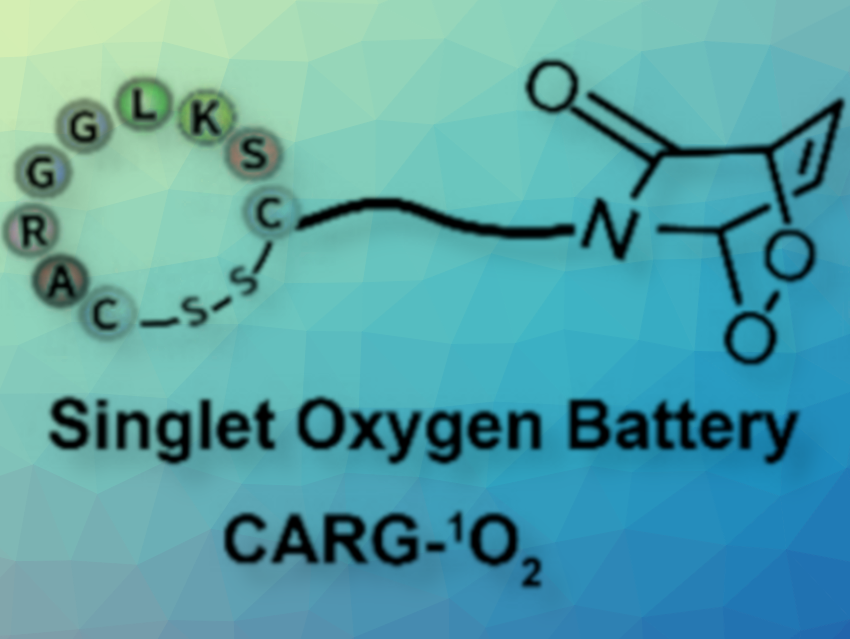
CARG-Py consists of a pyridone that tightly binds the singlet oxygen. The reactive oxygen molecule then bridges two opposite vertices of the ring (endoperoxide) as seen in the picture. The system was designed using a specific peptide called “CARGGLKSC16” that targets S. aureus. This peptide is conjugated with a pyridone group, resulting in CARG-Py. The peptide specifically “recognizes” MRSA bacteria, so the molecular batteries accumulate around and in the bacteria and continuously release their singlet oxygen.
The bacteria are thus simultaneously attacked at many different locations, including their membrane, DNA, enzymes, and other proteins. This makes the development of resistance virtually impossible. When administered to mice through nebulization, the singlet oxygen battery was shown to be very effective in treating pulmonary infections caused by MRSA. Systemic side effects were not observed.
- A Targeting Singlet Oxygen Battery for Multidrug-Resistant Bacterial Deep-Tissue Infections,
Yiwen Zhu, Minzheng Gao, Mengrui Su, Yanzhe Shen, Kai Zhang, Bingran Yu, Fu-Jian Xu,
Angew. Chem. Int. Ed. 2023.
https://doi.org/10.1002/anie.202306803