Diabetes is caused by a lack of insulin production by the pancreas. There is currently no cure, leaving patients to rely on external supplies of insulin or treatments to alter levels of blood glucose. The research, led by Dr. Tomoko Kuwabara, AIST Institute, Tsukuba, Japan, focuses on developing methods for defining human stem cell differentiation – the process through which cells can be adapted to a specialized role – for use in cell replacement treatments.
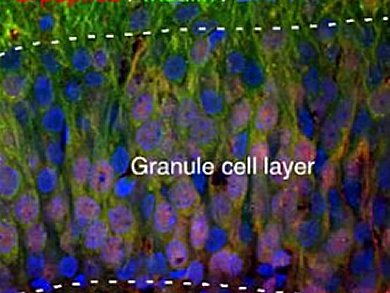
The hippocampus and olfactory bulb, at the front of the brain, provide an easily accessible tissue source for cells that could be transplanted directly into the pancreas. Normally neuronal cells do not produce high levels of insulin, pancreatic cells do. Once they had been transplanted into diabetic rats the cells not only started to express several key characteristics of pancreatic beta cells, but insulin production was increased and blood glucose levels were reduced.
The removal of the transplant increased levels of blood glucose, revealing that transplanting neural stem cells into the pancreas could be an effective treatment for diabetes.
- Insulin biosynthesis in neuronal progenitors derived from adult hippocampus and the olfactory bulb,
Tomoko Kuwabara, Mohamedi N. Kagalwala, Yasuko Onuma, Yuzuru Ito, Masaki Warashina Kazuyuki Terashima, Tsukasa Sanosaka, Kinichi Nakashima, Fred H. Gage, Makoto Asashima,
EMBO Molecular Medicine 2011.
DOI: 10.1002/emmm.201100177 - Accompanying Closeup
Neural stem cells for diabetes cell-based therapy,
Onur Basak, Hans Clevers,
EMBO Molecular Medicine 2011.
DOI: 10.1002/emmm.201100178